Abstract

Introduction:
Patients with unprovoked venous thromboembolism (VTE) have a high recurrence risk, and, according to guidelines, should receive extended oral anticoagulation (OAC). OAC prevents recurrence in most patients but may cause major bleeding. Patients with a low recurrence risk could therefore benefit from limited OAC duration. The Vienna prediction model (VPM) estimates the recurrence risk of patients with a first unprovoked deep vein thrombosis (DVT) of the leg and/or pulmonary embolism (PE) based on the patient's sex, site of index VTE and D-Dimer measured after stopping OAC (Eichinger et al., Circulation 2010). In a prospective cohort management study, we evaluated whether the VPM can identify patients with an unprovoked VTE at low recurrence risk.
Methods: The study was performed between January 2013 and May 2021 at two tertiary Austrian hospitals. Patients >18 years with a first symptomatic DVT of the leg and/or symptomatic PE were eligible. The diagnosis of VTE was established by compression ultrasonography (CUS), spiral computed tomography, or lung scanning. We excluded patients with previous VTE, VTE provoked by a temporary risk factor including surgery, trauma, pregnancy, immobilisation, or female hormone intake, with cancer, OAC duration longer than 7 months or OAC for reasons other than VTE. OAC was discontinued 3 to 7 months after VTE diagnosis. D-Dimer was measured by a quantitative assay 3 weeks later and the probability of recurrence was estimated by the VPM. In patients with <180 risk points (corresponding to a predicted one-year recurrence risk of <4.4%), OAC was not resumed. CUS of both legs was performed at the time of discontinuation of OAC for reference baseline imaging in case of suspected recurrence. Patients were seen after 3, 12 and 24 months or at recurrence. Patients with a high recurrence risk (>180 VPM risk points) were excluded and their management was left to the discretion of their local practitioner. The main outcome measure was independently adjudicated recurrence of symptomatic DVT of the leg and/or symptomatic PE.
The study was approved by the local ethics committees and all patients gave written informed consent.
Statistical analysis:
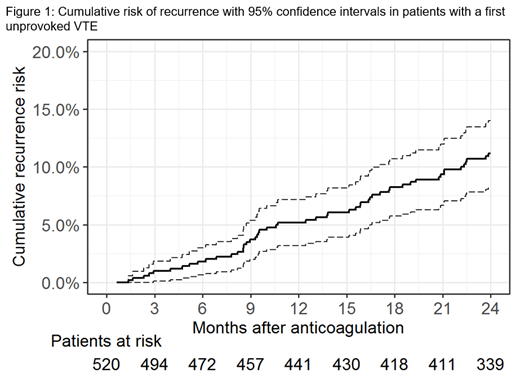
Baseline characteristics of patients were described by median and interquartile range (IQR) or by absolute frequency and percentage. The cumulative risk of recurrent VTE after discontinuation of OAC was estimated using the Kaplan-Meier method. Recurrence risk was also predicted with the VPM for each patient, and predictions were averaged over the study group.
Results:
Of 818 eligible patients, 520 (65%) had a risk score of <180 points and were classified as being at low risk of recurrence. They were included in the study and did not resume OAC. Their median age was 52 (42-65) years, and 289 (56%) were men. 226 (43%) patients had PE, 206 (40%) proximal and 88 (17%) distal DVT as index VTE. Median duration of anticoagulation was 3.9 (3.3-5.7) months, and the median time of follow-up was 23.9 (23.8, 23.9) months. Ten (1.9%) patients were lost to follow-up.52 patients (of which 30 were male) had non-fatal recurrent VTE (5.8 events per 100 patient-years, 95% CI 4.4-7.7). 28 (54%) patients had PE, 17 (33%) proximal and 7 (13%) distal DVT at recurrence.
The cumulative risk of recurrence at one and two years was 5.2% (95% CI 3.2-7.2) and 11.2% (95% CI 8.3-14), respectively (Figure 1). The corresponding predicted recurrence risk for the study group was 4% and 7%, respectively.
Conclusion: The VPM identifies patients with unprovoked VTE at low risk of recurrence. Applying the VPM refines risk stratification which could facilitate treatment decisions on the duration of OAC for patients and physicians. The model was well calibrated at one year. The apparent underestimation of the recurrence risk at two years could be countered by recalibration.
Eichinger: Takeda: Speakers Bureau; Daiichi-Sankyo: Speakers Bureau; BMS: Speakers Bureau; Bayer: Speakers Bureau; Pfizer: Speakers Bureau; Boehringer-Ingelheim: Speakers Bureau; CSL Behring: Speakers Bureau.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal